Moderate Scoliosis
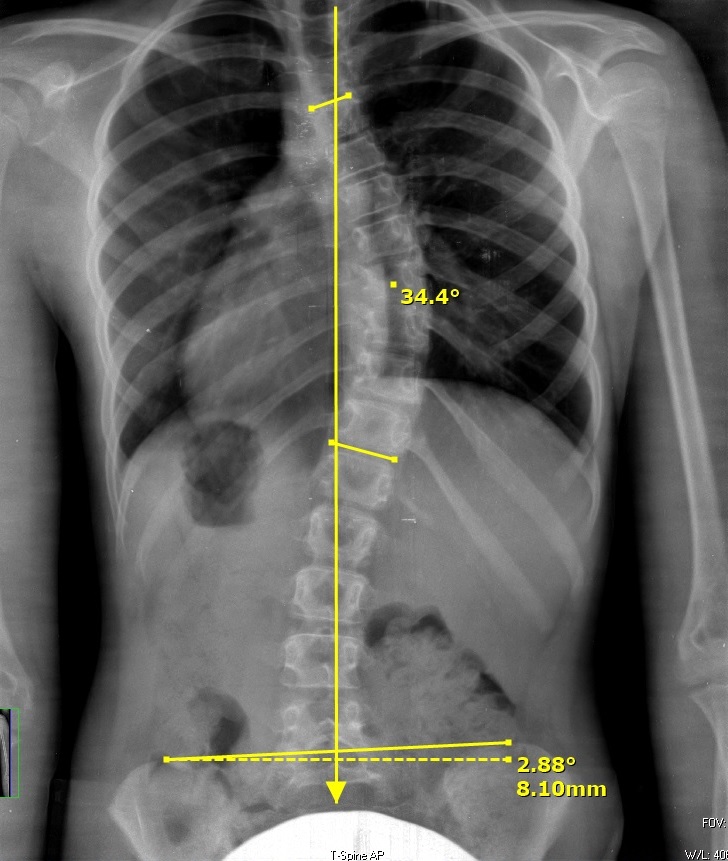
Moderate scoliosis refers to a more pronounced curvature of the spine, falling within a specific range of 25-50 degree Cobb angle measurements. Understanding this condition and the available treatment strategies is essential for individuals diagnosed with moderate scoliosis and their families. This web page provides valuable information on the Cobb angle measurement for moderate scoliosis, conventional treatment options, and the age groups typically affected by this condition.
Age Group Typically Affected
Moderate scoliosis can affect individuals of various age groups, but it is most commonly diagnosed during adolescence. It often manifests during growth spurts, between the ages of 8 and 13. During this period, rapid skeletal growth can lead to the progression of scoliosis. However, moderate scoliosis can also develop in adulthood, particularly as a result of untreated or progressive mild scoliosis. Regular spinal screenings during childhood and adolescence are crucial for early detection and timely intervention.
Conventional Treatment Strategies for Moderate Scoliosis
Observation: In cases of moderate scoliosis where the curvature is not rapidly progressing or causing significant symptoms, close monitoring may be recommended. Regular check-ups and X-rays are conducted to assess the curvature’s stability and determine if any intervention is necessary.
Bracing: Bracing is a common treatment approach for moderate scoliosis, particularly during the adolescent growth phase. A brace, typically worn for several hours a day, helps to halt or slow down the progression of the curvature by applying corrective pressure to the spine. The specific type of brace and duration of wear depend on individual circumstances and the recommendations of the healthcare provider.
- Surgical Intervention: In some cases, surgical intervention may be considered for moderate scoliosis. Surgery is typically recommended when the curvature exceeds 50 degrees, is rapidly progressing, or causes severe symptoms. The surgical procedure, known as spinal fusion, aims to correct and stabilize the curvature using metal rods and screws, along with bone grafts.
Conventional Vs. ScoliSMART Treatment
Conventional
Vs.
ScoliSMART
Mild Scoliosis
Mild Scoliosis
Moderate Scoliosis
Moderate Scoliosis
Conventional bracing is a widely used treatment approach for moderate scoliosis. The most commonly used conventional scoliosis braces are the Boston brace and the Wilmington brace. Both braces are symmetrical non-customized braces that have been used for several decades to try to prevent or slow the progression of scoliosis, not to improve it.
Typically, the brace is worn for 18 to 23 hours a day, with regular breaks for activities such as bathing and physical exercise. Compliance with the prescribed wear schedule is essential for the brace to be effective in controlling the progression of the spinal curvature.
ScoliSMART treatment involved a whole-body approach to care. Diagnostic testing is performed to assess the patient’s risk for curve progression, identifying various genetic and environmental risk factors. Based upon the current age and growth stage of the child, many different possible therapies may be employed, including the patented ScoliSMART Activity Suit (SAS), ScoliSMART BootCamp, and even more advanced kinds of customized 3D scoliosis bracing such as a Cheneau brace or other Cheneau variants, as well as nighttime-only bracing like a Providence brace. Any combination of these treatment may be used in order to achieve the best clinical outcome possible: curve improvement.
Severe Scoliosis
Severe Scoliosis
Scoliosis fusion surgery is a surgical procedure used to treat severe cases of scoliosis where the curvature of the spine is significant, typically exceeding 50 degrees on the Cobb angle measurement. It involves the fusion of vertebrae using bone grafts, metal rods, screws, and other fixation devices to correct the curvature and stabilize the spine. While the procedure can be highly effective in reducing or eliminating the spinal curvature, it is important to be aware of the potential costs, side effects, and complications associated with this surgery.
While scoliosis fusion surgery is generally safe, it is important to note that, like any surgical procedure, there are potential short-term and long-term complications that can arise. These can include:
Infection: There is a risk of developing a surgical site infection, which can be managed with antibiotics and proper wound care.
Blood loss: During surgery, there is a possibility of significant blood loss, requiring blood transfusion in some cases.
Nerve damage: There is a small risk of nerve damage during the surgical procedure, which can lead to weakness, numbness, or tingling in certain areas of the body.
Instrumentation failure: Rarely, the rods, screws, or other fixation devices used to stabilize the spine may shift, break, or fail to provide the desired correction, requiring further surgical intervention.
Nonunion or pseudarthrosis: In some cases, the fusion may not completely heal, resulting in a condition known as nonunion or pseudarthrosis. Additional surgery may be required to address this complication.
Rare complications: These may include deep vein thrombosis (blood clot), pulmonary embolism, adverse reactions to anesthesia, or allergic reactions to surgical materials.
- Restricted Spinal Mobility: Scoliosis fusion surgery involves permanently fusing segments of the spine using bone grafts, rods, screws, or other fixation devices. This fusion aims to halt the progression of the curvature and provide stability. However, the fusion also limits the mobility of the fused spinal segments. While the loss of mobility in the fused region may not significantly impact day-to-day activities for many individuals, it is important to recognize that flexibility and range of motion in the fused segments will be permanently reduced.
- Adjacent Segment Degeneration: Fusion surgery places increased stress on the adjacent vertebrae and discs in the spine, potentially leading to accelerated degeneration of those segments over time. This phenomenon is known as adjacent segment disease. The development of adjacent segment degeneration varies among individuals and can lead to symptoms such as pain, stiffness, and decreased function in the adjacent spinal segments. Regular follow-up and monitoring are important to detect and address any potential issues that may arise in the adjacent spinal segments.
- Spinal Implant Issues: The hardware (e.g., rods, screws) used during scoliosis fusion surgery can occasionally cause problems. Over time, the implants may become loose, migrate, or break. In some cases, additional surgery may be required to address these implant-related complications.
Newer types of scoliosis surgery have emerged as alternatives to conventional scoliosis fusion surgery, offering potential advantages such as preserving spinal flexibility and reducing the need for extensive fusion. Three notable examples of these newer surgical approaches are anterior scoliosis correction, vertebral body tethering, and ApiFix.
Anterior scoliosis correction involves accessing the spine through the front (anterior) of the body, as opposed to the traditional posterior (back) approach. This approach allows direct access to the vertebrae, discs, and ligaments, enabling more precise correction of the spinal curvature. During the procedure, the surgeon may remove or manipulate intervertebral discs and utilize specialized implants, such as screws, rods, or flexible tethering devices, to realign and stabilize the spine. Anterior scoliosis correction is associated with potentially reduced surgical trauma, faster recovery times, and improved preservation of spinal mobility.
Vertebral body tethering, also known as fusionless scoliosis surgery or growth modulation surgery, is a procedure primarily performed on skeletally immature adolescents with scoliosis. Instead of fusing the vertebrae, this approach uses flexible tethers (such as a flexible cord or tape) to guide the growth of the spine while maintaining spinal flexibility. The tethers are attached to the convex side of the spinal curvature, applying tension to modify the growth pattern and gradually correct the curvature over time. Vertebral body tethering offers the potential advantage of allowing continued spinal growth and preserving motion segments, potentially reducing the long-term impact on spinal flexibility and function.
ApiFix is a minimally invasive surgical system used to correct scoliosis in selected cases. It involves implanting a small, internal device that is attached to the spine. The device acts as a dynamic rod that provides continuous correction and stabilization of the spinal curvature. ApiFix is designed to allow controlled spinal movement while correcting the abnormal curvature during daily activities. This procedure is typically indicated for certain types of adolescent idiopathic scoliosis with specific curve patterns. It offers the potential benefits of reduced invasiveness, shorter operative times, and faster recovery compared to conventional fusion surgery.
It is important to note that while these newer surgical approaches show promise, they may not be suitable for all types of scoliosis or all patients. Each procedure has its own indications, considerations, and potential limitations. Remember, just because a curve reaches 50 degrees, it does not necessarily mean that surgery is required. Many patients with severe scoliosis receive tremendous benefit from non-surgical treatment options, such as the ScoliSMART Activity Suit, which allow them to maintain a healthy quality of life with minimal impact or pain.